The outermost layer of the eye is called Cornea. It is one of the essential components of the human eye as it allows the light to enter into the eye for us to have vision. A cornea is generally 12mm in length and 11mm in height. The cornea also contributes towards around 70 percent of the focusing power of the eye. That is the main reason why it is imperative to take care of the corneas.
Refractive problems like myopia, hyperopia, and astigmatism are caused due to a change in the shape of the cornea.
Structure of the Cornea
There are five layers of the cornea which have different functions:
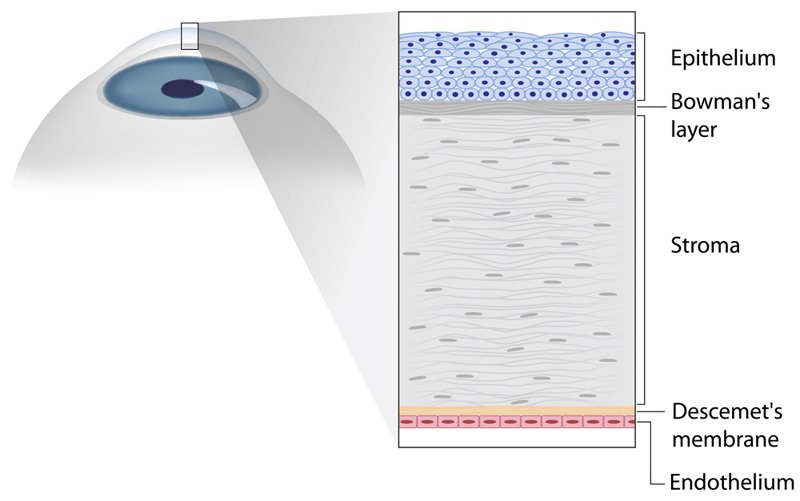
Epithelium – Keeps the Eye Healthy
It is the outermost layer of the cornea which means that whatever external objects will come in contact with the eyes, they will have to pass the epithelium. It is made up of regenerative cells which constantly shed and keep regenerating from time to time. It has two primary functions:
- It keeps away the dust, debris, water, bacteria and any other type of problem causing impurities from the eyes.
- Its smooth surface absorbs essential nutrients and oxygen from our tears.
Bowman’s Layer – Protects the Eye
It is also known as anterior limiting membrane and is made up of protein fibers which are called collagen. It is a strong layer that is between the epithelium and the corneal stroma and is built to protect the stroma.
Stroma – Gives a Perfection for Clarity
It is the middle layer of the cornea and contributes towards around 90 percent of the overall thickness of the cornea. It comprises mainly of collagen fibrils and water along with interconnected keratocytes which are used for the repair and maintenance of the cornea. There are 200 to 300 layers of collagen fibrils are arranged in a parallel manner, and this is the main reason that enables the cornea to be entirely transparent.
Descemet’s Membrane – Protects from Infection
It is the fourth layer of the cornea which is quite thin but very strong as it helps protect against any infections or injuries. It is also known as a posterior limiting membrane. It is also made up of collagen fibrils and separates the stroma from the corneal endothelium.
Endothelium – Maintains the Fluids
It is the final layer of the cornea which is in the innermost part. It is made up of mitochondria-rich cells. Bathed by aqueous humor, the endothelium’s primary function is to keep a perfect balance between the fluids flowing in and out of the cornea at all times. It is the layer that comes directly in contact with the iris and pupil of the eye.
Keratoconus – Most Common Problem Affecting the Cornea
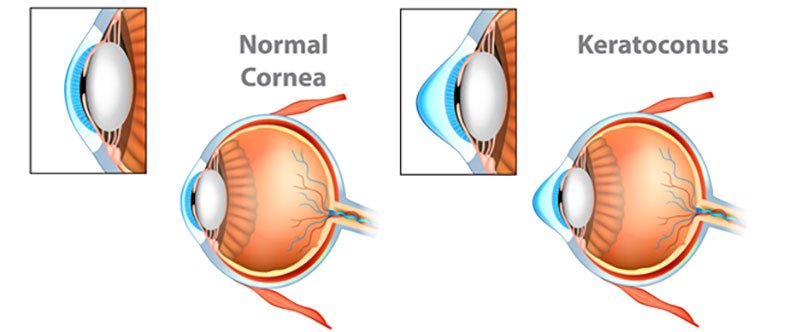
Keratoconus is a progressive disease of the eye in which the cornea becomes thin and begins to bulge into a conical shape. This results in irregular refraction of light rays entering the eye, resulting in blurred, distorted vision and a high astigmatic error (high cylindrical power of glasses).
It usually affects both eyes, although only one eye may be affected initially.
This usually starts at the time of puberty and progression rate is greatest in young people. Progression slows down in the fourth decade and is unusual after 40 years.
It is most commonly an isolated sporadic disorder or could manifest secondary to constant eye rubbing due to allergic eye disorders such as vernal keratoconjunctivitis during childhood.
What are the symptoms?
The patient’s symptoms could be variable depending on the stage of Keratoconus.
In early cases, patients usually complain of frequent change of glasses, increase in the refractive error especially astigmatism and inability to see 20/20 (6/6) vision despite using corrective glasses.
In advanced cases there is significant distortion of the images with profound visual loss.
Investigations to detect Keratoconus?
Keratometry can be used to detect keratoconus; however, corneal topography (Scheimpflug technology-Pentacam) has become indispensable in the management of keratoconus.
Pentacam is useful in detecting early keratoconus, following its progression and contact lens fitting.
Anterior Segment Optical Coherence Tomography (ASOCT) has also largely supplanted ultrasonic pachymetry to detect thickness of the cornea and the corneal epithelium.
What is the treatment?
Step 1 – Halting the progress of Keratoconus
Corneal Cross-Linking (C3R or CXL): Corneal collagen cross-linking is useful in halting the progression of the disease. This is popularly known as C3R or CXL which is a new therapeutic non-surgical treatment with a much higher success rate than conventional treatments. In this procedure, your surgeon uses riboflavin drops and exposes the eye to controlled ultraviolet radiation which makes the cornea stronger, and helps flatten it.
It is useful especially in adolescents who have the highest risk of progression.
There are various techniques of CXL depending on the patient’s corneal thickness. In corneal thickness > 400micron standard epi-off technique with isotonic riboflavin is performed using standard Dresden protocol or accelerated CXL.
In thinner corneas, various modifications are made such as use of hypo-osmolar riboflavin, contact lens assisted CXL, stromal lenticule assisted CXL, or customized thin cornea protocols.
Step 2 – Rehabilitation of Vision after halting the progress of Keratoconus
Spectacles & Contact Lenses
For visual rehabilitation, spectacles are useful in mild keratoconus. However, due to compromised visual quality and sub-optimal vision, most patients are unsatisfactory with the spectacles.
Contact lenses provide the advantage of masking the irregular corneal surface and thereby providing dramatic improvement in the visual acuity in most cases.
Rigid gas permeable (RGP) lenses, hybrid lenses, Rose-K lenses, mini-scleral and scleral lenses are some of the commonly used lenses in keratoconus.
Surgical Intervention
INTACS, Corneal Inserts or Intracorneal Ring Segments: In patients who are contact lens intolerable or in patients who does not want to wear contact lens but need better visual quality with spectacles, intrastromal corneal ring segments (INTACS), which look like half-moon shaped clear plastic rings, could be useful.
Single or double INTACS rings could be placed in the mid-peripheral cornea depending on the patient’s topographic and refractive parameters.
This procedure does not prevent progression; however, this could help to regularize corneal surface and centre the cone thereby improving the corrected visual quality or contact lens tolerance.
This procedure could be combined with CXL to prevent progression.
T-CAT, Topography-guided Custom Ablation Treatment: It could be used in the management of keratoconus to modify the corneal anatomy using excimer laser.
This procedure attempts to improve the central corneal symmetry rather than correction of the patient’s refractive errors, thereby altering minimal corneal tissue of up to 50 microns. This procedure is done after removal of the corneal epithelium using phototherapeutic keratectomy (PTK). Hence, T-CAT could result in improvement of the corneal topography and corrected distance visual acuity.
This procedure could also be combined with various CXL protocols.
ICL, Phakic Intraocular Lenses: ICLs are micro thin lenses implanted over the natural lens, inside the eye, to correct spectacle power.
They are similar to contact lenses placed in eyes except that a contact lens is temporary and has to be put on a daily basis whereas ICL is put inside the eye permanently.
It is a viable option for visual rehabilitation if the Keratoconus patient requires independence from spectacle or contact lenses.
Eyes having CXL or C3R tend to have a fluctuation in refraction in the initial post-treatment. After the refraction stabilizes (may take up to 3 months), these patients may be offered ICL surgery.
Toric ICLs are especially useful in patients with astigmatism.
Keratoplasty (Corneal Transplantation): In cases of patients with severe scarring in the visual axis or advanced keratoconus with progressive thinning with unstable contact lens fit and poor visual acuity, eye doctors prefer to replace the cornea with a donated cornea, the surgery is called Keratoplasty.
Depending on the extent of scarring and corneal thickness, your surgeon may decide to perform a full thickness procedure called Penetrating Keratoplasty (PK), or a partial thickness procedure called Deep Anterior Lamellar Keratoplasty (DALK).
Cornea Surgery & Keratoconus treatment in Delhi at Eye7 Chaudhary Eye Centre
At Eye7 Chaudhary Eye Centre, we deal with a lot of problematic corneal cases on a daily basis. We have expert surgeons who have numerous years of experience in dealing with various diseases related to the cornea and their impact on the overall health of a person’s eye.
We are fully equipped with the state of the art equipment to perform each of the above mentioned advanced Keratoconus treatments.
After the initial discussion with the patient, our doctors evaluate the complexity of the case and suggest a solution as per the situation and the budget of a patient. If there seems to be a need, the patients can go with the option of a cornea surgery or Keratoconus treatment to maintain the overall health of the eye as well as to make sure that the infection does not extend to the other parts of the face and body.








